The College has received questions from occupational therapists about the Standard for Psychotherapy, 2023. This Psychotherapy Q&A resource was developed in consultation with the College’s Practice Subcommittee and occupational therapists practicing psychotherapy to help answer these questions.
If you would like to further discuss any questions, please contact the Practice Resource Service.
Defining Psychotherapy in Occupational Therapy Practice
Occupational therapists should reflect and analyze their own practice (i.e., considering client factors, role, competencies, techniques used and practice setting) to determine if they are practising psychotherapy. Psychotherapy involves developing a therapeutic relationship with a client where specific psychotherapeutic approaches are applied to collaboratively assess and address a client’s thoughts, emotions, and/or behaviours. Practising psychotherapy is not an entry-level skill and requires additional education and supervision.
Various modalities are used by occupational therapists in psychotherapy practice. A few examples include Exposure Therapy, Cognitive Behavioural Therapy (CBT), Cognitive Processing Therapy (CPT), Dialectical Behavioural Therapy (DBT) and Acceptance and Commitment Therapy (ACT). An example in practice would be an occupational therapist using Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) or components of TF-CBT with a client whose experience of trauma limits their daily functioning and occupational engagement.
This is not an exhaustive list as occupational therapists may develop competencies in other techniques and modalities.
All occupational therapists practising psychotherapy are expected to follow the Standard for Psychotherapy, 2023 (coto.org).
The Standard for Psychotherapy does not apply when occupational therapists are providing general mental health services.
Occupational therapy mental health services enhance a client’s performance and mental health by enabling participation in occupations linked to overall well-being. Providing mental health services requires general occupational therapy knowledge, skill, and judgment, although certain approaches might require additional training.
Mental health techniques include activity analysis, skills training, goal setting, health coaching, psychoeducation, supportive listening, motivational interviewing, wellness recovery planning, and relaxation strategies. Psychoeducation (from the College’s perspective) involves providing general education and information regarding mental health, symptoms and psychotherapy modalities.
An example of mental health services would be an occupational therapist who is teaching organizational skills to a client with ADHD symptoms that is interfering with school-related occupations.
Yes, occupational therapists can use a combination of modalities and techniques depending on the context and needs of each client. For instance, an occupational therapist may offer general mental health support to a client by providing psychoeducation. In addition, they may use psychotherapeutic approaches such as cognitive behaviour therapy (CBT) to address specific functional limitations. When components of psychotherapy are used, the Standard for Psychotherapy applies.
Controlled Act
Controlled Acts are procedures or activities which may pose a risk to the public if not performed by a qualified practitioner. The Regulated Health Professions Act, 1991 (RHPA) added psychotherapy with clients who have a serious disorder of thought, cognition, mood, emotional regulation, perception or memory to the list of controlled acts in 2007. The legislation grants occupational therapists the authority to perform the controlled act of psychotherapy.
The controlled act of psychotherapy is defined in section 3.1 (1) of the Occupational Therapy Act, 1991 as “to treat, by means of psychotherapy technique delivered through a therapeutic relationship, an individual’s serious disorder of thought, cognition, mood, emotional regulation, perception or memory that may seriously impair the individual’s judgement, insight, behaviour, communication or social functioning.” The requirements for occupational therapists performing the controlled act are defined in the Ontario Regulation 474/19: Controlled Acts and set out in the College’s Standard for Psychotherapy.
Psychotherapy is broad in nature. This definition may only describe a portion of an occupational therapist’s psychotherapy clients as they may provide psychotherapy to clients with less serious disorders outside the controlled act. The College made the decision that psychotherapy carries risks to clients whether it falls within the definition of the controlled act or outside the controlled act. Accordingly, the Standard for Psychotherapy applies to all occupational therapists practising psychotherapy. Psychotherapy Examples
| Example | |
|---|---|
| Controlled Act of Psychotherapy | An occupational therapist provides treatment for a client recently diagnosed with post-traumatic stress disorder. This client’s occupational participation has been seriously impacted such that they are on a leave of absence from their work as a first responder, are experiencing marital stress and have withdrawn from other social relationships. The occupational therapist is trained in psychotherapy techniques and uses these (such as the therapeutic use of self, cognitive behavioural therapy, and exposure therapy) as part of the intervention plan. All components of the definition of the controlled act of psychotherapy are present. The Standard for Psychotherapy applies. |
| Psychotherapy Outside the Controlled Act | An occupational therapist enters an arrangement with a client diagnosed several years ago with bipolar disorder. The client is currently not in an active episode and their occupational performance is not seriously impaired. They are seeking psychotherapy to continue their recovery and improve the relationship with their partner. The occupational therapist is trained in psychotherapy techniques and uses behavioural, cognitive and emotion focused techniques including the therapeutic use of self as part of the intervention plan. The client’s current level of impairment does not meet the definition of the controlled act; however, psychotherapy is being provided. The Standard for Psychotherapy applies. |
The College has only collected data about the number of occupational therapists who are performing the controlled act of psychotherapy.
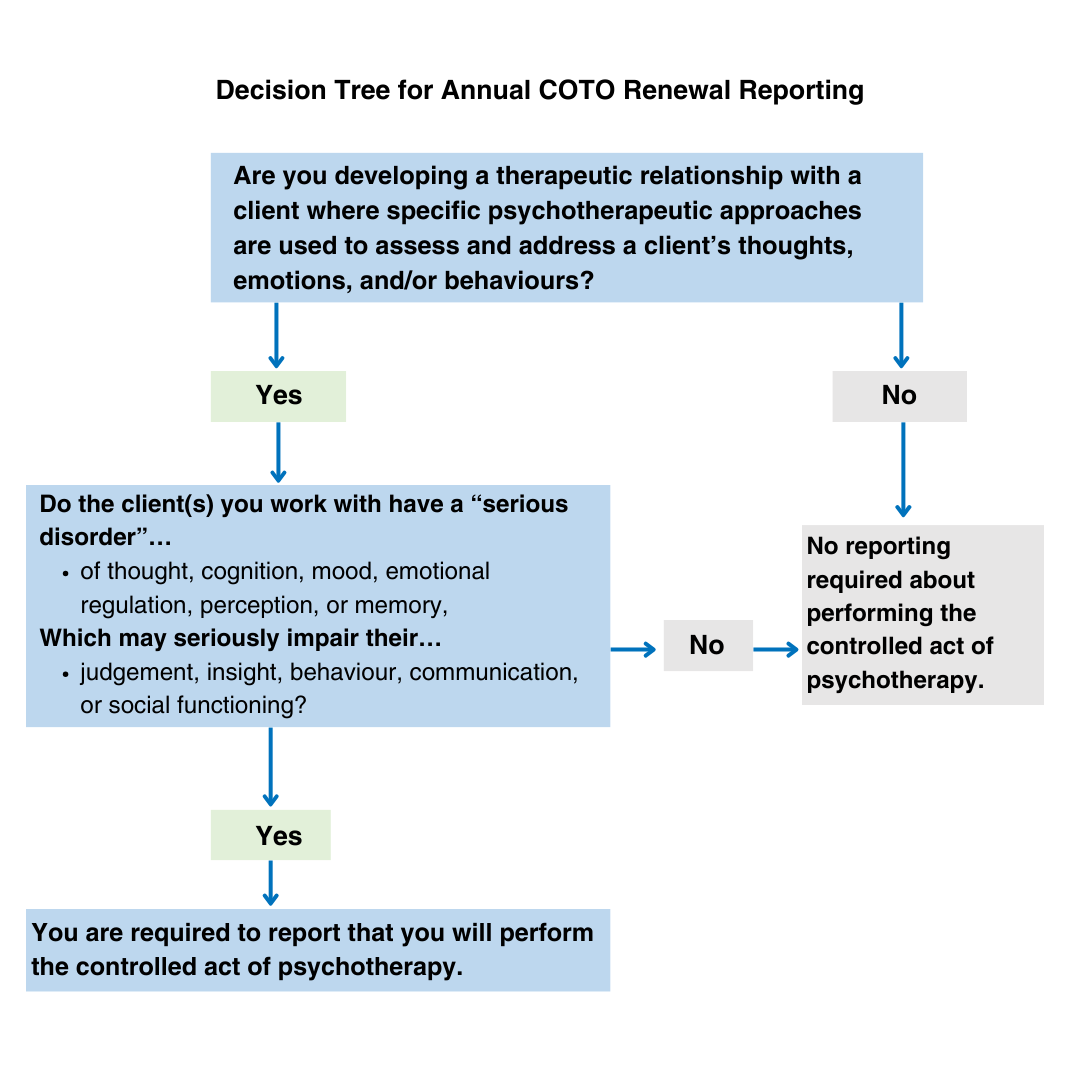
The following decision-tree can be used to help you determine whether you are performing the controlled act of psychotherapy for the purpose of reporting on annual renewal.
Training and Supervision
Occupational therapists are expected to obtain psychotherapy training that has these components:
- instructional (instructor led, not self-taught),
- theoretical (based on psychotherapeutic theories), and
- practical (involves supervision).
Pairing supervision with instruction and theoretical training allows for the practical application of theory to practice. Continued competence may be obtained through workshops, professional networks, literature reviews, and quality improvement initiatives.
Psychotherapy training and supervision requirements at a glance:
Instructional and Theoretical Educational Training
- Select training that is appropriate for the occupational therapist’s learning needs, client needs, evidence-informed approaches, scope of services, previous training and experience, comprehensiveness, and relevance.
- In the beginning, training components provide a foundational understanding of psychotherapeutic modalities (e.g. certificate programs).
- Later, engage in workshops, professional networks, literature reviews, and quality improvement activities to continue developing competence.
Practical Supervision
- A formal supervision arrangement; long-term commitment occurring at regular intervals.
- Recommended minimum of 50 hours of supervision over at least the first 2 years of psychotherapy practice. This may extend longer for OTs who are not working full-time.
- The supervisor and supervisee must develop a supervisory agreement composed of
- Administrative details (e.g., start and end dates, meeting frequency)
- Responsibilities of both parties
- Confirmation of accountability for client services
- Emergency processes and plans
- Both supervisor and supervisee must keep supervisory or meeting notes.
Psychotherapy supervisors must be experienced in psychotherapy, competent to provide supervision, and eligible to perform the controlled act. Supervisors must be active registrants of at least one of the following regulatory bodies:
- College of Nurses of Ontario
- College of Occupational Therapists of Ontario
- College of Physicians and Surgeons of Ontario
- College of Psychologists of Ontario
- College of Registered Psychotherapists of Ontario
- Ontario College of Social Workers and Social Service Workers
You can connect with your employer, other psychotherapy practitioners or organizations to determine whether they can offer supervision or can connect you with other qualified psychotherapy practitioners who are available to support a supervisee.
Another option is to contact professional associations that support members authorized to practise psychotherapy. For example, the Ontario Society of Occupational Therapists has an online search tool for this purpose.
The Canadian Association of Occupational Therapists may also have psychotherapy practitioners registered in Ontario who are willing to offer supervision.
Occupational therapists who are considering supervising, should self assess and reflect on their competency to supervise another therapist. The occupational therapist must determine whether they are competent in their psychotherapy practice (including performing the controlled act) in order to provide supervision. At a minimum, occupational therapists must meet all training requirements set out in the Standard for Psychotherapy, 2023.
Occupational therapists can supervise other regulated healthcare professionals that are permitted to practise the controlled act of psychotherapy in Ontario. The occupational therapist supervisor must be experienced and competent to supervise. They must also be aware of the supervisory requirements and criteria of the supervisee’s regulatory body and determine if they are able to provide the supervision outlined by the supervisee’s College.
Registrants from the following 6 regulatory bodies are permitted to practise the controlled act of psychotherapy:
- College of Nurses of Ontario
- College of Occupational Therapists of Ontario
- College of Physicians and Surgeons of Ontario
- College of Psychologists of Ontario
- College of Registered Psychotherapists of Ontario
- Ontario College of Social Workers and Social Service Workers
Upon completing 50 hours of supervision, the occupational therapist and supervisor can decide whether to maintain formal supervision or shift to a consultation-based approach with a mentor, colleague or peer.
Occupational therapists should continue to engage in workshops, professional networks, literature reviews, and quality improvement initiatives to maintain competence and stay current on evidence-based practice.
| Scenario | Do I need formal supervision? |
|---|---|
| I had a psychotherapy supervision agreement in place before the updated Standards came into effect on June 1st, 2023. Do I have to start over with obtaining 50 hours? | No. The supervision hours that an occupational therapist acquired prior to June 1st, 2023, can count towards the 50 hours. Supervision time previously accumulated should be reflected in supervisory meeting notes which would be used to confirm their supervision if requested. |
| I have been practising psychotherapy for the past 5 years. Do I need formal supervision again? | No. An occupational therapist with 5 years of psychotherapy experience would have been accountable to the supervision requirements under the previous Standard, and likely has already acquired 50 hours of supervision. They would not be expected to start over with formal supervision again. They may have shifted to a consultative approach at this point. The occupational therapist should be able to produce documentation to confirm their supervision if requested. |
| I started practising psychotherapy 15 years ago before there was a Standard for Psychotherapy. What are my responsibilities now and do I need supervision? | No. Occupational therapists have always had a professional responsibility to obtain/maintain competence and engage in ongoing reflective practice via individual or group consultation. A therapist with 15 years of experience would likely have acquired 50 hours of supervision in varying formats and be engaged in a consultative approach at this point. If requested, the occupational therapist would be required to speak to their work and supervision model, training, competencies and experience and provide their rationale to support how they meet this expectation. |
| I have been providing only mental health services for many years. Do I need supervision? | No. For occupational therapists who are only providing general mental health services, the Standard for Psychotherapy does not apply. |
| I have been working in general mental health for 20 years and have started incorporating psychotherapeutic techniques in my practice. Do I need supervision even though I am very experienced in my field? | Yes. Before entering a new practice area like incorporating psychotherapeutic techniques, occupational therapists must obtain the appropriate training and the 50 hours of formal supervision to ensure they have the competencies to practise psychotherapy safely. The type of training and supervision may be tailored to the level of experience of the occupational therapist but the requirements under the Standard still apply. Mental health techniques can include activity analysis, skills training, goal setting, health coaching, psychoeducation, supportive listening, motivational interviewing, wellness recovery planning, and relaxation strategies. The Standard for Psychotherapy does not apply when occupational therapists are only providing general mental health services. |
Accountability
Occupational therapists should ensure that clinical accountability is discussed when arranging supervisory agreements. Members of other regulatory colleges may have a different understanding of “supervision” and “consultation”. Therefore, it is important that occupational therapists are clear that under COTO’s Standard, the supervisee remains accountable for the psychotherapy service provided to their clients.
COTO issues a general registration certificate to applicants who meet all the registration requirements. General registrants can practise in any area of occupational therapy without restriction if the expectations for competency are met.
The College’s position is that psychotherapy is not an entry-level occupational therapy skill. Therefore, provisional registrants are required to complete all their registration requirements and obtain the additional psychotherapy competencies through training and supervision to practise psychotherapy. Temporary registrants will need to obtain permission from the Registrar to practise psychotherapy.
Title Use
Using the title “Psychotherapist” is not mandatory when practising psychotherapy. An occupational therapist must always identify themselves by using the title “occupational therapist”. This informs clients that they are accountable to COTO. An occupational therapist can choose to communicate to clients that they practise psychotherapy by using acceptable versions of title as outlined in the Standard.
For example,
- Jane Doe, OT Reg. (Ont.), Psychotherapist
- John Doe, OT Reg. (Ont.), Practising in Psychotherapy
Regardless of the title version used, the occupational therapist must be clear and transparent when discussing services with their clients, including when they are providing psychotherapy.
The Standard does not specify when occupational therapists can use the title “Psychotherapist”. Occupational therapists are advised to collaborate with their supervisors to determine when it is suitable to use the psychotherapist title by self assessment and reflection about their competency, formal training, theoretical understanding, and practical experience.
Occupational therapists are authorized to perform the controlled act of psychotherapy under section 27 of the RHPA. Occupational therapists are permitted to use the protected title ‘Psychotherapist’ when they identify themselves as an occupational therapist as set out in the section 33.1 (1) of the RHPA.
Psychotherapy techniques are considered higher risk interventions and are not an entry-level skill. The skills, knowledge, and judgment required to perform psychotherapy are developed over time. As such, the title of “Psychotherapist” may also be incorporated over time.
Occupational therapists must be mindful that the title “Psychotherapist” should not be utilized solely for billing or invoicing purposes.
Occupational therapists can be registered with more than one regulatory body. It is not a requirement for occupational therapists practising psychotherapy to be registered with the CRPO, however if dually registered, they are accountable to and must fulfill obligations of both Colleges. For example, occupational therapists would be required to adhere to both College’s Standards of Practice and Quality Assurance requirements. Occupational therapists must be clear and transparent to their clients about their dual accountabilities, and it must be clear to the client when they are receiving occupational therapy services. Occupational therapists must also indicate they are registered with another regulatory body at annual COTO renewal.
Funding Insurance
Occupational therapists can follow up with the professional associations (for example, Ontario Society of Occupational Therapists, Canadian Association of Occupational Therapists) who advocate on behalf of the profession.
For any questions, please contact our Practice Resource Service at 1-800-890-6570 ext. 240 or practice@coto.org.